Voice disorders in adults
Voice disorders in adults
Voice disorders are a range of conditions that affect the larynx (voice box). They can cause changes to the voice called dysphonia or loss of voice called aphonia. These changes can affect the way the voice sounds, for example, making it sound hoarse, croaky, strained, breathy or weak. Voice disorders can also make the throat feel different, for example it might feel tight, sore, achy or dry.
Bradford Voice Therapy service
The voice team in Bradford works closely with the Ear, Nose and Throat (ENT) Department at Bradford Royal Infirmary to assess, diagnose and treat voice disorders. You will be supported to understand your voice difficulties and be given advice and techniques to improve voice quality, enable optimum voice use and prevent future problems.
Assessment
You will be assessed by a member of the ENT (ear, nose, throat) Department at either Bradford Royal Infirmary or at one of a number of specialist clinics in the Bradford area. If appropriate you will then be referred to the voice therapy team or to the combined voice clinic.
Combined clinics with both an ENT consultant and voice therapists present take place three times a month at Bradford Royal Infirmary. At these clinics your progress is reviewed and then further management options discussed.
Voice therapy
Voice therapy is usually on an individual basis and takes place at one of two community clinics in Bradford. Therapy includes:
- helping you understand how your voice works
- helping you understand the specific difficulty you are experiencing, and
- advice on vocal hygiene – how best to look after your voice and throat.
Therapy may also include exercises and techniques designed to reduce discomfort and help the voice to work more efficiently.
The number of sessions required varies from patient to patient. The team also runs voice therapy workshops usually comprising six to eight participants which take place on a Monday evening from 4.30pm until 6.00pm at Westbourne Green Community Health Care Centre in Bradford.
How do you access our service?
- Visit your GP if you have a problem with your voice who, if necessary, will refer you for an ENT (ear, nose, throat) appointment.
- After the ENT appointment you will be referred to the Speech and Language Therapy Voice team if appropriate.
You will be given an individual appointment at which your difficulties will be discussed and advice and further treatment options agreed upon.
Useful information and resources
You may find the information and resources below useful.
-
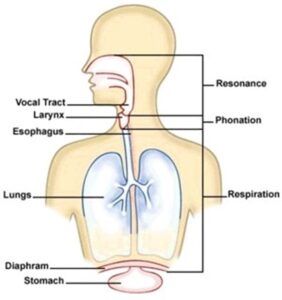 Breath (respiration) – this is the ‘fuel’ or power source for the voice. We take a breath in and when we want to make a noise the air moves up the windpipe and through the voice box.
Breath (respiration) – this is the ‘fuel’ or power source for the voice. We take a breath in and when we want to make a noise the air moves up the windpipe and through the voice box.- Phonation (making the sound) – the vocal cords come together to vibrate. The vibration chops the air flow to produce a voice.
- Resonance – the sound created at the level of the vocal cords is shaped by the movements of the throat and oral cavity (including the lips, tongue, palate, and jaw) to create speech.
-
How to avoid irritating the lining of the voice box
Many things can irritate the lining of your voice box, so try to avoid these:
- smoking – stop if you can or cut down
- chemical irritants or dry, dusty, smoky conditions
- fumes, including strong deodorants, perfumes, paints or household products
- eating a large meal before going to bed at night – acid indigestion, alcohol and spicy foods could trigger reflux. If you suffer from this frequently, take some medication, for example Gaviscon Advance.
How to avoid straining the muscles of your voice box
- To avoid straining your voice box muscles, try not to
- cough or clear your throat harshly
- whisper
- talk loudly or shout above the noise at social or sports events, or over the sound of the radio or TV
- spend excessive amounts of time talking on the phone
- sing when your throat is hurting or sing at a pitch level that is not comfortable.
More tips
- If you have to use the telephone for your living, try to have regular breaks
- Think about what you drink: too much alcohol, coffee, tea or cola can dry you up
- If you use asthma inhalers, make sure you use a spacer if possible and gargle after use
- Life stresses and anxiety can add to tension in the voice box. Make time for yourself and find ways to relax
What can help
- Drink six-eight glasses of water daily, or sip water throughout the day if you find that difficult.
- Don’t clear your throat unnecessarily. Try to suck a sweet or chew teeth-whitening gum. Or try a gentle huff and swallow or sniff and swallow to clear your voice.
- Warm up your voice if you’re going to use it for a long time.
- Try inhaling steam regularly to hydrate the vocal cords
- Rest your voice frequently. It can be helpful to use a gentle volume (“confidential” voice or “library” voice is often helpful)
Other things to note
- Hormonal changes (such as the menopause, pregnancy or menstruation) can affect voice quality.
- The voice is closely linked with emotion, so tension or depression might show in your voice.
- Get medical advice if you’re worried, especially if your voice sounds different for more than two weeks.
-
What is acid reflux?
Your stomach contains strong digestive acids and enzymes that digest your food. Sometimes the acid and enzymes can to travel up from the stomach into the food pipe. This can cause the symptoms of indigestion and heartburn. The medical term for this is gastro-oesophageal reflux (GOR).
Sometimes, small amounts of stomach acid can come up as far as the throat and voice box. The medical term for this is laryngopharyngeal reflux (LPR). It is often called ‘silent reflux’ as many people do not experience any symptoms.
Acid reflux can occur during the day or night, even if a person hasn’t eaten anything.
What is acid reflux like?
These may vary but some of the most common symptoms of silent reflux are:
- a feeling of food sticking in your throat
- feeling a lump in your throat
- a hoarse, tight or ‘croaky’ voice
- clearing your throat a lot
- difficulty swallowing (especially tablets or hard and sticky foods)
- a sore, dry and sensitive throat
- occasional unpleasant ‘acid’ or ‘sickly’ taste at the back of the mouth
- a feeling of mucus/phlegm collecting in your throat
- sudden coughing or choking at night
- a cough that may last for days and weeks
- a lot of burping, particularly during the day.
What can I do to reduce acid reflux?
These are things you can do to reduce silent reflux and indigestion:
- Lose weight and eat a healthy diet
- Eat less fried foods, spicy foods, chocolate and citrus juices. Eat smaller portions of these foods if you have them
- Give up smoking
- Raise the head of your bed four-six inches (place blocks under the legs/base of the bed at the head end)
- Leave three hours between eating and lying down
- Bend at the knees when you pick things up
- Wear loose clothing around your waist
- Chew whitening gum after meals
- Eat smaller meals more regularly
- Eat slowly, chewing each mouthful well
- Avoid fizzy drinks and caffeine – Try caffeine-free versions and drink water or herbal teas instead
- Drink less alcohol, especially before bed
You can take one-two teaspoons of Gaviscon Advance 15-30 mins after meals and before going to bed. This will stop the stomach acid from coming out and will cool and protect your food pipe.
You may have been prescribed an antacid tablet such as Lansoprazole. You should take this 30 minutes before either your breakfast or evening meal or both if you have been prescribed two a day.
Always take the advice of your GP and/or Speech and Language Therapist before starting to take new medication or altering the dose of medication you already take.